Around one in 90 women in the UK experience an ectopic pregnancy, and most of those take place in the fallopian tubes.
Unfortunately, in the unlikely event that you do get pregnant with a coil, there is a raised risk of an ectopic pregnancy, which means the embryo cannot grow.
I had my second copper coil, otherwise known as an Intra Uterine Device, in 2018.
I had come back from an epic hike round the Pyrenees – a mountain range in the south of France. We had driven down there to explore the area and walk the five day “Pass’Aran” route.
When my period did not arrive, Google reassured me that this could be caused by low progesterone (hormone) levels, which could be caused by “extreme exercise”.
Then I had sore breasts, and once again Google said this was due to low progesterone levels, but as I was also feeling a bit more tired than usual, I checked with a pregnancy test.
Pregnant.
It didn’t say Not Pregnant. It must be a mistake.
1-2 weeks (it confusingly showed 2-3, but this meant weeks since conception which the leaflet explained was 1-2 weeks pregnant).
So it was early. I walked around swearing, head in hands. What was I going to do?
Did I want it? It was so inconvenient – we were in the process of buying a house, my boyfriend works away, we were going to New Zealand…now was not the time.
But I could not kill something that was both of us and I could not kill something I really wanted. Yes it wasn’t the right time but when was?
I didn’t have time to process, I had to get to work.
But I had to get dressed first and find the few bigger clothes I’d bought from another time I temporarily gained weight.
I wondered who to tell. Should I tell anyone but Jonny?
Maybe Jonny wouldn’t want it and then there’s the shame of abortion, so I wouldn’t tell anyone. I didn’t want anyone judging me.
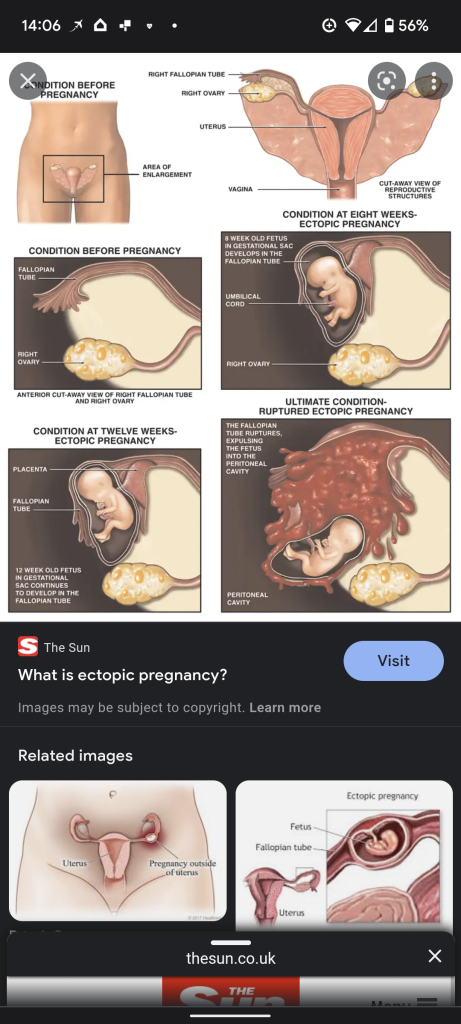
I couldn’t keep it in and I needed emotional support, so I confided in a close friend and it really helped. Her cousin had had an ectopic pregnancy it turned out, and they had also found out at six weeks. She had her fallopian tube removed, as the embryo can damage it. At least we are born with two.
Before seeing the GP I wanted to talk to Jonny – then I could ask for an abortion as well as a scan if needed. He was shocked and froze but he wasn’t annoyed or upset as I expected. He said we should see what was going on with it first, before we made a decision. Ever the pragmatist.
“Is that the only one you did?”
“No, it’s the third.”
“Oh………Is there anything else that could make it test positive?”
“No Jonny!”
The next morning I contacted the GP first thing and filled in an online form. Almost immediately I was text with the first appointment of the day. I explained how I’d started spotting instead of a period and then how my breasts had become sore and that as of Thursday night, it looked like I was having a period.
The doctor examined me and referred me to the Gynae Accident and Emergency department at the local hospital for a scan (my second time as an emergency patient in a year). She said to make sure Jonny was with me and to tell Gynae if I had symptoms that would suggest even more of an emergency, like pain or heavy bleeding.
After an hour of waiting at reception, the nurse did a safeguarding and general information interview. “From your dates you’d be six weeks pregnant” she said.
She took me round for a urine and blood test and after waiting for ages, I had a scan.
I was excited as I held my boyfriend’s hand down the corridor, wondering how he’d feel when he saw our baby.
“Do you want me to show you the embryo if I can find it?” the nurse asked.
“Yes please” I replied. “Jonny, do you want to see it?”
“Yes” he said, looking both excited and confused.
I had read that an embryo of six weeks sent out an electrical signal that sounds like a heartbeat on a scan. It would be the size of a pomegranate seed and look like a tadpole.
I waited to hear the signal.
There was silence and a lot of prodding. It was uncomfortable but didn’t hurt.
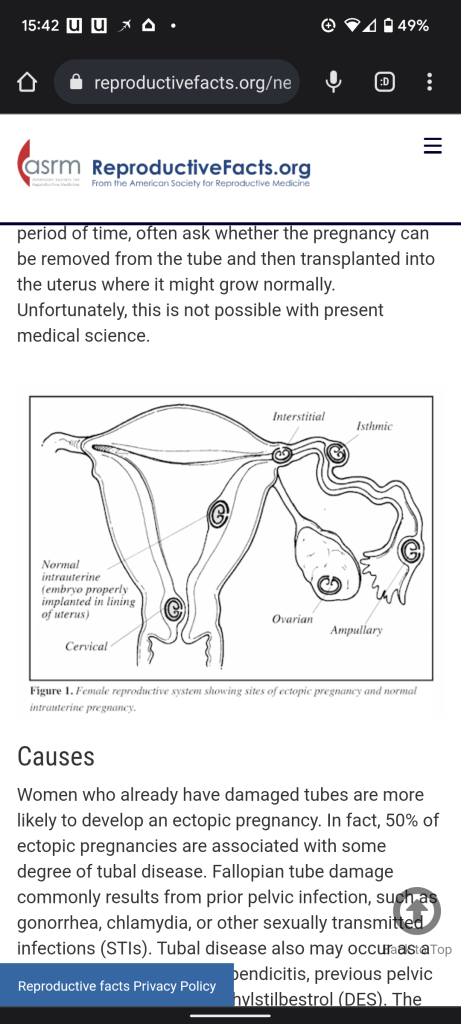
“I’m very sorry to tell you this, but I can’t find a pregnancy in your uterus. I can confirm that it’s likely to be an ectopic pregnancy, which means it’s growing outside of your uterus.” I was devastated.
“It’s growing next to your ovary.”
“Next to the ovary?? outside the uterus?? not on the ovary then??”
“Do you want to see?”
“Yes please”.
The nurse rotated the screen and there was the dark space of my ovary and then a dark space next to it that looked like a comma stuck to my ovary. I couldn’t make out any details as it was grainy.
“I can’t be certain, but that may be the sac there.”
It was so strange to see, but it made it feel more real and I was glad for that, as it helped me to accept that this was really happening, and I needed to get my head around it.
Not only was I pregnant, but it could not continue. I knew logically that was good as it was the wrong time for us, but it didn’t make it feel any better emotionally.
How? why? why me?
I then waited two more hours for the blood test results.

Jonny came up with lunch. I felt sorry for the other pregnant ladies, who had also been waiting hours. One woman had an overweight partner who was snoring loudly and continuously falling off his chair. He hadn’t got her any lunch, but if he did there was a risk that he wouldn’t hear what the nurse had to say. I wondered why they didn’t have a ticket system, like they did with blood tests.
The doctor called me in, finally.
He explained about the pregnancy hormone they had measured for. I replied “oh yes, Human Immunoglobulin something…”
“yes, that one. It’s at 500. We need to wait and see what happens, because there is a still a chance that you are pregnant in the uterus and we can’t see it, as it is so early.”
“But I thought there was a mass?”
“Yes, but that could just be a cyst.”
“So we will have you back in in two days to see what has happened. If it doubles it is likely to be in your uterus. If it doesn’t then we can confirm an ectopic pregnancy.”
My treatment options were:
- Expectant management – waiting to miscarry (and hoping I didn’t die from a ruptured fallopian tube).
- Have an injection to stop the cells growing, and make them reabsorb into the body (genius).
- Have my fallopian tube removed with keyhole (laparoscopic) surgery (also genius, but less chance of getting pregnant in future).
I felt fortunate that as of the 1980s, option 2 had also become available. The drug was previously only used in cancer treatment but has no bad side effects. Also, keyhole surgery has drastically reduced the time you need to spend in hospital – you can leave the same day instead of being on bed rest for weeks.
Google informed me that 500 HcG was the average reading for five weeks of a pregnancy in the uterus.
Dame Laura Kenny, the Olympic medal-winning cyclist, has recently spoken out about her ectopic pregnancy experience and this is why I’m blogging about it – it helped me to read about other women’s experiences.
I was relieved that hospital was done with. I had a missed a day of work and I was emotionally drained.
When I got home I lay on the sofa for a while, but life goes on, I had a night out with the netball girls.
Turns out you can’t enjoy alcohol pregnant – it just made me feel sick.
And so did a Dr Pepper can and a frangipani almond croissant. I didn’t like salad before, but now I want lots of dark leafy green salad and steak. Your body craves what it needs.





You must be logged in to post a comment.